Dawn Phenomenon.
It sounds innocuous, doesn't it?
Dawn... That time when light gently filters through the window, peeking through the cracks in the curtains. Birds sing. The occasional early morning commuter's car rolls by. A gentle turn of the body in bed to get a few more precious moments of sleep. You can hear Morning Mood by Grieg, can't you?
Phenomenon... It's just, like, this thing that happens, man... </TheDude>
The reality - waking with blood glucose levels in hyperglycemic range. Here are the symptoms I experience:
- Vice-like headache
- Powerful need to urinate
- Dry mouth, eyes, nose... all mucus membrane areas. Yes, even there.
- Joint and muscle ache and inflammation
- Fatigue
For some PWD, this is an occasional thing. For me? Every. Single. Day.
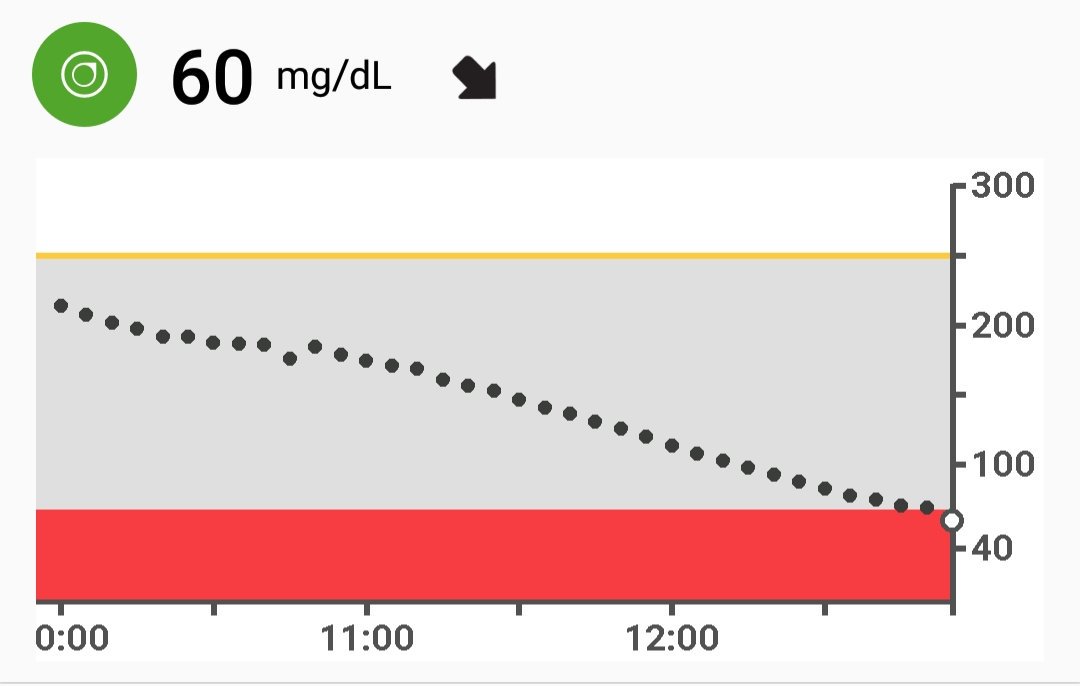
This is what it looks like in a CGM representation. This was my morning on 05 Jul 18.
 For the non-T1D folks, here's what you're looking at:
For the non-T1D folks, here's what you're looking at:Ideal range for people with T1D is 70 mg/dl to 130 mg/dl. At night, the lower bound raises to 80 mg/dl to have a safety buffer in the event of the basal (background) insulin use profile causing a dip.
The upper limit is lowered overnight to prevent waking up with the symptoms of hyperglycemia.
For most PWD, Dawn Phenomenon isn't a thing. If their basal injection or pump rate is correct, they'll have that relatively flat line that you see between 0100 and 0400 all night long. Whatever they went to sleep at, they'll wake up +/- 25 mg/dl.
And then there's people like me...
I usually get about 6-7 hours of sleep a night. I fall asleep sometime between 1 and 2 am and wake between 7:30 and 9 am.
Last night, I was running high until about midnight due to a high carb/high fat lunch and dinner. The correction dose I took around 11pm kicked in fully a little after 1am.
In a 'normal' diabetic (hahahahaha!) this would have resulted in a waking BGL somewhere around 100-120 mg/dl.
I have finally realised that the sheer exhaustion I wake up with every day is the reason I tend towards afternoon naps. Part of it is that I am just tired by then, since the overnight sleep wasn't restful. The other part of it is that it's the one time I sleep where I generally don't wake out of range.
What's the solution?
- Some people have had success with zero-carbs after 4pm.
- Others only have relief from being able to set differing basal rates by time with an insulin pump.
- Some people have had luck with the more modern basal insulins (Toujeo, Tresiba).
- Some people on MDI (multiple daily injections) set an alarm and inject a correction dose before the rise happens and go back to sleep.
But the good news is that it looks like my basal dosage is good for the times when my body isn't busy telling me "I made you glucose, HERE!"